|

|
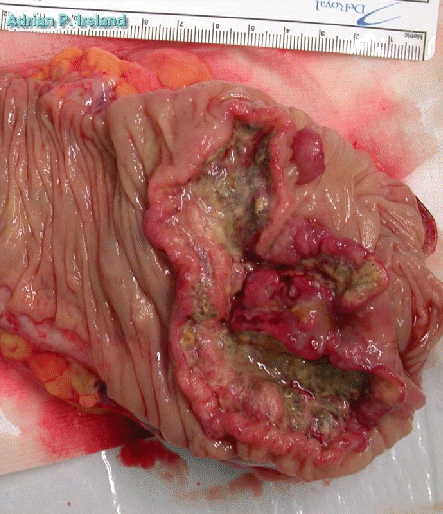
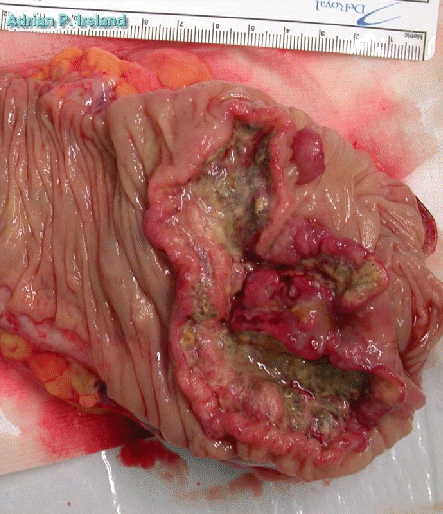
The surgical procedure of choice for a tumor of the caecum is a right hemicolectomy.
Some surgeons advocate a medial approach with primary control of the blood vessels, following control of the blood vessels the colon is mobilised, this is popular in Franch. Others advocate a lateral approach with control of the blood vessels after the colon is mobilised, this approach is popular in Ireland.
The main lymphatics supplying the caecum accompany the ileo-colic artery. Thus resections with the intent of removing these lymphatics must remove the ileo-colic artery and some of the terminal ileum must be resected. The right colic artery is also resected with its lymphatics.
| Right ureter |
| Gonadal Vessels |
| Duodenum |
In mobilising the right colon, the surgeon divides the peritoneal attachments to the terminal ileum and caecum. This incision is carried along up the ascending colon to the hepatic flexure. As the colon is reflected medially the surgeon must be careful to stay anterior to Gerota's fascia which surrounds the kidney. The gonadal vessels and ureter should be pushed back into the retroperitoneum and not included in the specimen. On the anterior and medial kidney in the upper part of the disection the surgeon must take care not to damage the second and third parts of the duodenum. The inferior vena cava is behind the duodenum and the portal vein anterior to the third part before it enters the pancreas with the superior mesenteric artery. The duodenal `C' loop encloses the head of the pancreas.
The terminal ileum and the transverse colon are divided. The transection line in the ileum is usually oblique, with the shortest end being the end away from the mesentry, this is because there is a greater blood supply on the mesenteric side. Sufficient terminal ileum is resected to remove the blood vessels with their lymphatics. Note however, that if too much ileum is resected the patient runs the risk of developing vitamin B12 deficieny and cholerrheic diarrhoea.
The ileum is anastamosed to the transverse colon either by hand or with a stapling device. Neither appears to be superior to the other.
If the surgeon opts for a stapled ileo-transverse anastamosis, this is most commonly done with the GIA stapler which will form 4 lines of staples which are split in half by an in-built blade, this leaves two lines of staples on each side. The surgon makes a short enterotomy in the antemesenteric border of the ileum about 1 cm proximal to the transected end (which has been stapled shut). A similar short colotomy is made about 1 cm distal to the cut end of the transverse colon (which has also been stapled shut). The two loops of bowel at put side by side, with the antemesenteric borders meeting. The stapling device is introduced through the enterotomy and colotomy and closed to bring the loops together, the stapler is fired forming a side to side ileo-transveres anastamosis. The surgeon then closes the hole through which the stapler was introduced, either with another stapler or with some sutures. The hole in the mesentry is closed to prevent the formation of internal herniae.
If the surgeon opts for a hand sewn anastamosis, he may form it in a somewhat similar fashion to the side to side stapled anastamosis described above. It is just as easy however to form an end to end anastamosis. The ileum is cut obliquely across as described above, but if the colon is very large the cut in the ileum can be lengenthened. The ileum and colon and sewn together taking bites that are close together on the ileum and further apart on the colon. This then approximates the diameter of the colon to the ileum.
